Cancer Genetics
Birt-Hogg-Dubé syndrome is a genetic disorder caused by mutations to the FLCN gene, whose job is to control cell division. Most commonly, people with Birt-Hogg Dubé syndrome face an increased risk of developing kidney cancer; however, it can also increase the risk of other cancers of the urinary tract.
Cowden syndrome is a rare genetic disorder that occurs due to mutations to the PTEN gene. People with Cowden syndrome have an increased risk for developing many types of cancer, but the risk of developing breast cancer among women is greatest. Women with Cowden syndrome have a 50% to 85% likelihood of developing breast cancer in their lifetime and oftentimes, they develop their breast cancer at a younger age. The risk of developing thyroid cancer, kidney cancer, and endometrial (or uterine) cancer is also quite high among people with Cowden syndrome.
These patients can also develop hamartomas, which are benign growths of the skin, uterus, breast, gut, and thyroid. Multiple hamartomas in various organs, a big head, and specific skin sores known as trichilemmomas and acral keratoses are all signs of this syndrome. But only genetic testing can confirm the mutation that causes Cowden syndrome.
Familial adenomatous polyposis is a genetic disease caused by changes in the APC gene. It is characterized by polyps — sometimes thousands — which are benign growths inside the colon, rectum, and other parts of the intestinal tract. There is a chance that the polyps can become cancerous and spread throughout the body.
People with familial adenomatous polyposis have a much higher risk of developing colon cancer. They also have an increased risk of developing bile duct cancer (cancer of the tubes that carry bile from the liver to the gallbladder), stomach cancer, pancreatic cancer, medulloblastoma (brain cancer in children), hepatoblastoma (liver cancer in children), and thyroid cancer.
Gorlin syndrome is caused by mutations to either the PTCH1 or SUFU genes, which are responsible for stopping the growth of tumors.
Gorlin syndrome is associated with palmoplantar pits (small depressions in the palms or soles of the feet), benign cysts in the jawbone that can hurt and swell, and multiple basal cell carcinomas (a type of skin cancer).
In inherited and familial cancers, genetic mutations that cause cancer are usually passed down from one or both parents. These mutations can increase a person’s risk of developing cancer and can affect various organs and tissues in the body. Some common examples of inherited or familial cancers include breast cancer, ovarian cancer, colorectal cancer, and pancreatic cancer. It is important for individuals with a family history of cancer to speak with their health care provider about genetic counseling and testing and get regular screening for early detection and prevention of cancer.
About 5-10% of cancers result from an inherited genetic mutation. Most inherited cancer types are caused by defects in the genes that regulate healthy cell growth and division. These genes are called tumor suppressor genes. They help to prevent the development of cancer by correcting errors in DNA and slowing down or stopping the growth of cells that have the potential to become cancerous. When tumor suppressor genes are mutated or not functioning properly, cells can grow and divide uncontrollably, leading to the development of cancer. BRCA1, BRCA2, and TP53 are a few examples of tumor suppressor genes.
Certain factors increase the likelihood of a familial cancer syndrome, including the following:
- Many family members having the same type of cancer, especially if it is an uncommon or rare type of cancer
- Families where cancers occur at younger ages than usual — for example, a 20-year-old having colon cancer
- Instances when someone has more than one type of cancer, like a woman who develops both breast and ovarian cancer
- When cancers occur in both of a pair of organs in a person, like both eyes, both kidneys, or both breasts
- Certain childhood cancers, especially if more than one sibling develops cancer
- When cancer occurs in the sex not usually affected, like breast cancer in a man
- Cancer — even if the cancers are different types of cancer — occurring in many generations, like a grandfather, father, and son
When trying to determine if cancer might run in your family, it is important to collect as much information as possible about each case of cancer, such as who has (or had) the cancer. How old was the relative when diagnosed with cancer? What type of cancer is it or was it? Did the relative have more than one type of cancer? What is your relation to the affected person? Which side of the family is the relative on? Did the person who developed cancer have any known risk factors for his or her type of cancer? Additionally, it is important to determine if anyone in the family with cancer or without cancer had genetic testing, and if that testing showed any abnormal genes. Gathering this information prior to your appointment will make it more efficient. To make the process easier and even more efficient, at Mount Sinai, we will provide you with a questionnaire you are advised to complete prior to your visit.
Hereditary leiomyomatosis and renal cell cancer is a genetic disease caused by FH gene mutations. People with HLRCC get harmless growths called leiomyomas on the skin and in the uterus. Although it is not common, these benign lesions can become cancerous. People who carry an FH gene mutation are also at risk of developing kidney cancer.
This is a genetic disorder caused by changes in the RB1 gene, which increases the risk of a rare tumor of the eye. Retinoblastoma usually develops in children younger than 5. Parents may notice whiteness in the pupil of the eye (the black part in the middle of the eye), problems with eyesight, or lazy eyes.
Li-Fraumeni syndrome occurs when there are mutations to the TP53 gene. Like the BRCA1 and BRCA2 genes, the TP53 gene helps cells repair damaged DNA; however, if the gene is mutated, it does not do its job as well. Adrenocortical carcinoma, brain tumors, premenopausal breast cancer, osteosarcoma, soft tissue sarcoma, thyroid, colon, skin, lung, and leukemias are linked to LFS. There are guidelines for screening and surveillance specific to patients with LFS.
Lynch syndrome occurs due to changes in MLH1, PMS2, MSH6, MSH2, and EPCAM genes. Like many hereditary cancer syndromes, mutated genes cannot repair damage to DNA the way healthy genes can.
Lynch syndrome is associated with early onset colorectal cancer (before the age of 50). Lynch syndrome also increases a person’s risk of developing endometrial cancer, or cancers of the ovaries, stomach, liver, kidneys, brain, or skin. For people with Lynch syndrome, it’s important to have regular screenings for cancer, especially colonoscopies.
There are different types of multiple endocrine neoplasia caused by mutations to the MEN1, RET, and CDKN1B genes. These mutations result in cancers of the endocrine system. The endocrine system includes the glands that make hormones, so people with multiple endocrine neoplasia have an increased risk of developing adrenal, parathyroid, pituitary, pancreatic, and thyroid cancers.
This is a genetic disorder caused by MUTYH gene mutations that lead to multiple colon tumors and a higher chance of colorectal cancer. Ten to 100 polyps form in the colon and rectum that are harmless and not cancerous; however, they can become cancerous over time. Genetic testing can detect the affected gene in the carrier family members.
Neurofibromatosis results from mutations to the NF1 gene or NF2 gene. Regardless of which gene is affected, people with neurofibromatosis face an increased risk of benign and cancerous growths, some of which can be disfiguring. In addition, neurofibromatosis increases a person’s risk of several types of cancer, including eye tumors, brain and spinal cord tumors, and breast cancers.
PJS occurs when there are mutations to the STK11 gene. PJS is a very rare syndrome. People with PJS have an increased risk of developing cancer in multiple organs. Because of this, patients with PJS should get regular checkups and screenings for polyps and cancer, including colonoscopies, endoscopies, mammograms, ultrasounds, MRIs, physical exams, and blood tests.
Tuberous sclerosis is a genetic disease caused by mutations in the TSC1 or TSC2 genes. These genes tell cells how to make proteins that control cell division. People with tuberous sclerosis have a slightly increased risk of developing kidney and brain cancer.
In addition, they often develop benign growths in the eyes, skin, lungs, heart, kidneys, and brain. While they’re not cancerous, the growths can cause seizures, make it harder to see (when they’re in the eyes), and affect breathing and heart function (when they’re in the lungs or heart). Other symptoms include changes to the skin that look like pimples, thicker or bumpier skin, and lighter skin spots. Problems with behavior like violence, self-harm, restlessness, and issues related to thought and learning like ADHD, autism spectrum disorder, intellectual disability, or developmental delays are also common.
Von Hippel-Lindau syndrome is a genetic disease caused by mutations to the VHL gene. Patients have a higher chance of getting either benign (not cancerous) or malignant (cancerous) tumors. Cases are identified mostly between the ages of 12 and 35. Some common tumors associated with Von Hippel-Lindau syndrome include papillary cystadenomas (tumors in the genital tract), pheochromocytomas (tumors in the adrenal glands that are located on top of each kidney and make essential hormones), pancreatic cysts or cancer, kidney cysts or cancer, endolymphatic sac tumors in the inner ear that can cause hearing loss, and hemangiomas in the central nervous system and retina. Clear-cell kidney carcinoma is the most common type of cancer among people with Von Hippel-Lindau syndrome, affecting about 40% of people with the mutation. Many of the tumors linked to Von Hippel-Lindau syndrome are benign, which means they are not dangerous. However, they can lead to significant problems, like losing hearing (endolymphatic sac tumors) or having high blood pressure (pheochromocytomas).
Our Physicians
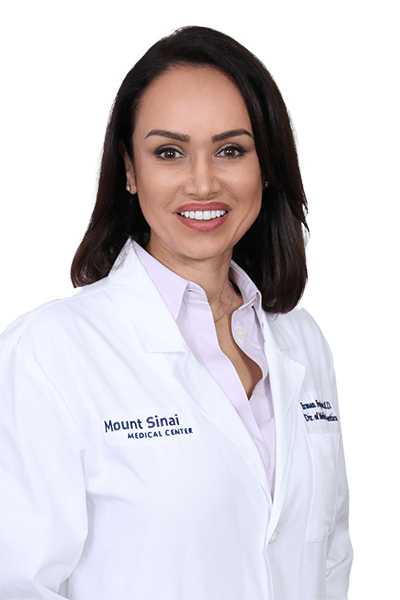
Irman Forghani, MD, FACMG
Director of Genetics at Mount Sinai Medical Center
- Medical Genetics
- Cancer
- Mount Sinai Medical Center (Main Campus)
- 305.535.1859