Mount Sinai Medical Center receives grant to conduct clinical trial testing stroke-prevention filter in high-risk heart surgeries.
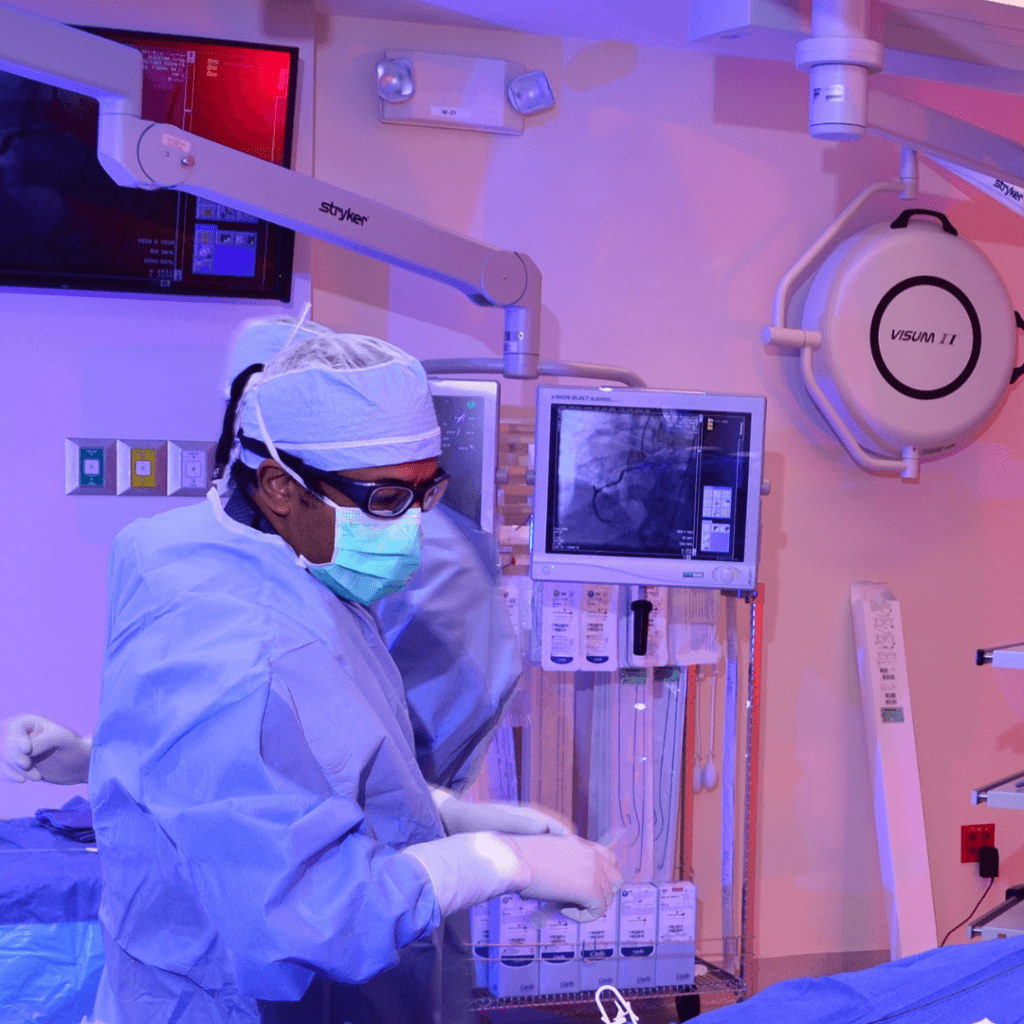
At the forefront of advancing research in cardiac procedures, Mount Sinai Medical Center is set to lead a groundbreaking clinical trial aimed at reducing stroke and cognitive decline in patients undergoing cardiac surgery. The Florida Heart Research Foundation has granted the medical center the necessary resources to conduct the trial, which focuses on evaluating the Sentinel CEP filter—an FDA-approved device designed to diminish embolic debris, specifically hardened heart valve fragments, which can break off and travel during transcatheter aortic valve replacements (TAVR). Dr. Beohar explains:
“In simple terms, when you do cardiac surgery, you are manipulating the aorta, which is the big artery that comes out of the heart,” Dr. Beohar explains. “Pieces of plaque can break loose from there or from the valve itself and go up to the brain. These travel through the carotid arteries.”
Starting in March, the study, officially titled “A Cerebral Embolic Protection During High-Risk Cardiac Surgery: A Feasibility Study of the Sentinel Cerebral Embolic Filter Device to Reduce Neurologic Complications,” will test 30 patients with specific risk factors, such as advanced age (more than 70 years old) or previous cardiac procedures.
The purpose of the Sentinel CEP filter is to gather debris as it travels upstream through the carotid arteries, the two major blood vessels that supply the brain. Positioned in these arteries, the filter prevents debris from advancing toward the brain and is removed at the end of the procedure, mitigating any potential health risks like a stroke.
“It is taught that the strokes and the cognitive decline after cardiac surgery may be similarly related because of small micro particles that break loose and get into the circulation of the brain and interfere with the blood supply there,” Dr. Beohar emphasizes. “Therefore, preventing this debris from getting to the brain may obviously reduce the risk of having a stroke as well as decrease the risk of cognitive decline afterwards.”
The study overall aims to determine a few things. First, it aims to evaluate the practicality of placing and retrieving the device in the operating room using a mobile X-ray imaging unit (C-arm), which is used for intra-arterial and intravenous equipment placement. Second, it aims to assess the ability to pathologically characterize debris collected in the filter, meaning figuring out exactly where the debris is coming from. Third, it aims to determine the frequency of embolic debris collection in the device. Finally, it aims to investigate the feasibility of conducting preoperative and 30-day postoperative neurological evaluations.
Dr. Beohar expresses optimism regarding the success of the trial, drawing on the medical center’s expertise in using the device during transcatheter aortic valve procedures.
“We expect that given our expertise in using the device doing transcatheter aortic valves that we should be successful also during cardiac surgery. And, if we are successful, which means that over 70% of these 30 patients get the filter placed and removed successfully, than we plan to expand this into a national study on a much larger number of patients undergoing cardiac surgery.”
The trial is estimated to last over a twelve-month timeline. There is currently no data studying the use of this device in cardiac surgery, and, thanks to the efforts of Dr. Beohar and his team, Mount Sinai will be the first to carry out this trial.
For more information on Mount Sinai’s approach to catheter-based interventions for cardiovascular procedures, visit https://www.msmc.com/medical_care/cardiovascular-care/catheter-interventions/.